Expertise in Eligibility Verification Services
Complete Revenue Cycle Management for
Medical & Dental
Clinics, Practices and Hospitals
- Shared Vision: Your Business is our Business
- Cloud Based Billing Software or Work on Yours
- Certified Coders: ICD 10 Coders, HIPPA and CDT
- Real Support with Dedicated Managers

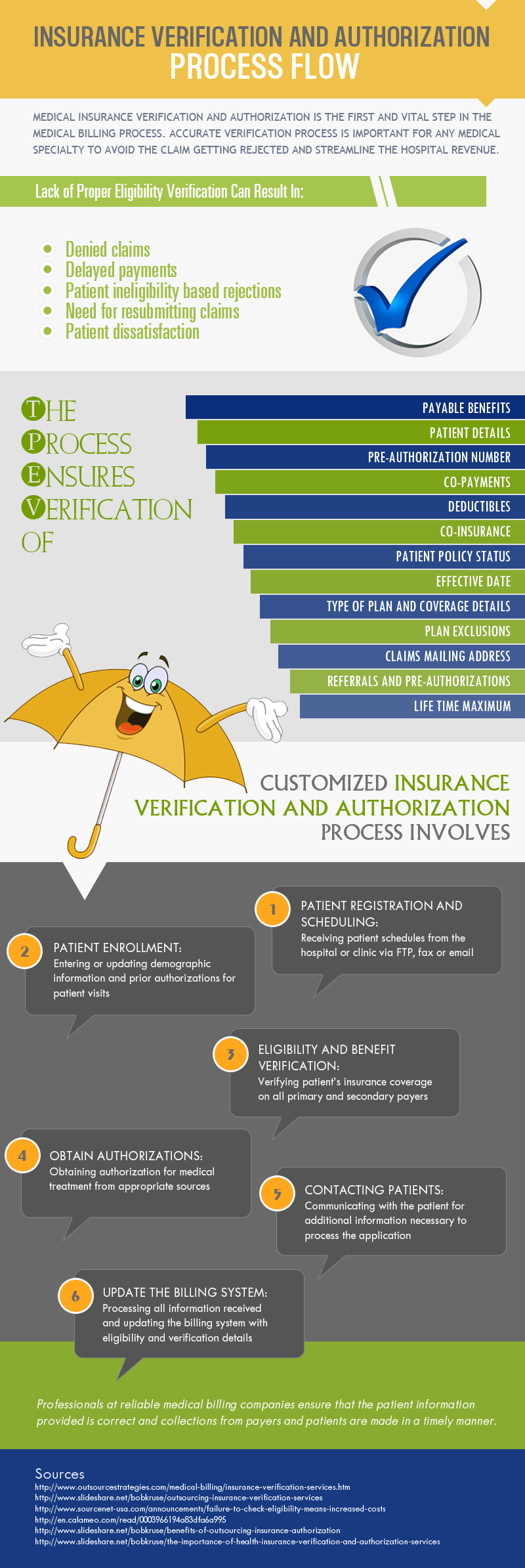
Eligibility Verification
Eligibility verification is one of the challenging tasks faced by healthcare facilities. This challenge has become even greater with changing insurance rules and guidelines, and the flood of newly insured patients and patients who are changing plans. To improve cash flow, physicians need to verify eligibility and benefit coverage before claim submission.
Comprehensive Eligibility Verification Process
More than just basic verifications, our services are all inclusive and much more robust. We can work with your software and login in via VPN or use our own billing software.
We receive schedules from the hospital via EDI, email or fax. Our team verifies all patient benefits based on the reason for the office visit. Instead of just relying on websites, we directly call up the carriers, and document and record the calls to save the practice crucial time.
Our team verifies:
- Co-pays
- Co-insurances
- Claims mailing address
- Deductibles
- Patient policy status
- Effective date
- Payable benefits
- Plan exclusions
- Health insurance caps
- Type of plan and coverage details
- Referrals and pre-authorizations
- Out of network benefits
- DME reimbursement
Our services cover specific codes, procedures, surgeries, drugs, Medicare Managed Care plans and more. When necessary, we call the insurance company and/or patients for detailed verification of insurance benefits. We also update your billing system with the information.
We can help with any type of insurance claims – No-Fault or Personal Injury Protection, Workers’ Compensation and Liability.
Why GreenLeavez?
Outsourcing your medical billing to GreenLeavez can save you up to 40% on your operational costs.
Call Our Toll-Free Number
To learn more about our medical billing and coding services or to discuss your requirements with our Solutions Manager.
GET YOUR FREE TRIAL TODAY!
