Insurance Authorization Services
Complete Revenue Cycle Management for
Medical Practices, Clinics and Hospitals
- Shared Vision: Your Business is our Business
- Cloud Based Billing Software or Work on Yours
- Certified Coders: ICD 10 Coders, HIPPA and CDT
- Real Support with Dedicated Managers

Insurance Authorization Services
Patient insurance verification and authorization plays a major role in a hospital’s claims denial management program. A leading medical billing outsourcing company, GreenLeavez has years of experience in providing insurance authorization service for diverse medical specialties. Serving all 50 states within the US, we verify coverage for all major and minor medical insurance plans in the country such as Blue Cross Blue Shield, United Healthcare, AETNA, GHI, Medicare and Medicaid, No-Fault, Workers’ Compensation and Liability.
Our insurance authorization company works as an extension of the client office every step of the way.
Benefit from our Free Trial Offer! Get a Free Solutions Consultation!
Comprehensive Insurance Verification Services
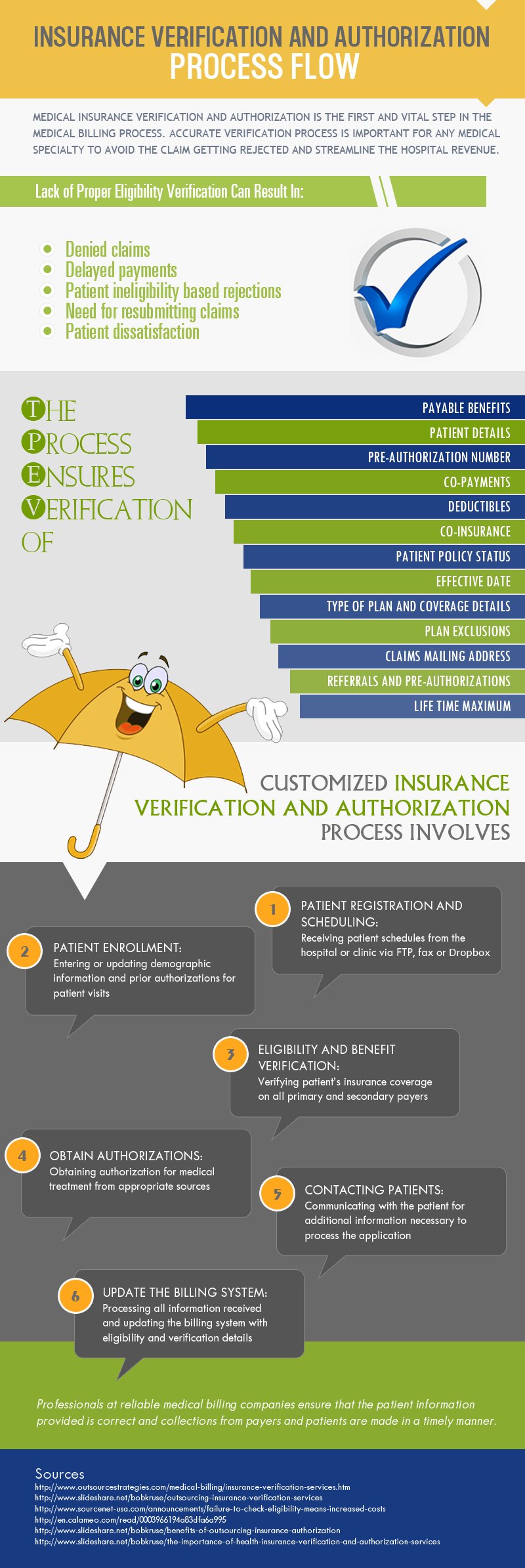
Our team of specialists completes all the benefit verification work well before the office visit and follow up with payers after the initial submission till confirmation is obtained. The service includes verification of all details such as:
- Payable benefits
- Co-pays
- Co-insurances
- Deductibles
- Patient policy status
- Effective date
- Type of plan and coverage details
- Plan exclusions
- Claims mailing address
- Referrals & pre-authorizations
- Health insurance caps
- DME reimbursement
Insurance Eligibility Verification
Our team of verification experts processes prior authorization requests for your patients quickly and efficiently. We are also experienced in authorizing up to 300 DME cases per day. We communicate with the concerned agencies/companies for appeals, missing information, and other matters.
Stay 3-5 Days Ahead Of Your Patient Visits!
Our Insurance Eligibility Verification Process

Patient Registration and Scheduling – Receiving patient schedules from the hospital or clinic via FTP, Fax or Dropbox. We can work directly on your practice management system.
Patient Enrollment – Entering demographic information entry or update
Eligibility Verification – Verifying coverage on all primary and secondary payers
Authorization – Confirming authorization for treatment from appropriate sources, if applicable
Contacting Patients – For further insurance details, we communicate with the patients
Billing System Update – Updating the billing system with the verified details
What Makes GreenLeavez Unique?
No long-term yearly contracts
Eligibility verification performed in batch and real-time
Benefits
Our team of experts has long-term experience in the industry and can assist in overcoming all your challenges. When you choose to outsource your insurance benefit verification and authorization services to us, you benefit from:
- Speedy approval and authorization
- Simplified workflow
- Reduced risk
- Reduced number of returned claims
- Faster billing cycles
- Minimal delays
- Improved payment and collections
- Free up your staff to focus on more productive tasks
An infographic presentation of the insurance verification process is given here.
Outsourcing your medical billing to GreenLeavez can save you up to 40% on your operational costs.
Call Our Toll-Free Number
GET YOUR FREE TRIAL TODAY!



