Health Insurance Verification and Authorization Process
Complete Revenue Cycle Management for
Dental Clinics, Practices and Hospitals
- Shared Vision: Your Business is our Business
- Cloud Based Billing Software or Work on Yours
- Certified Coders: ICD 10 Coders, HIPPA and CDT
- Real Support with Dedicated Managers
Contact GreenLeavez Today!
Ask about our free trial to see firsthand how our services can benefit your practice.

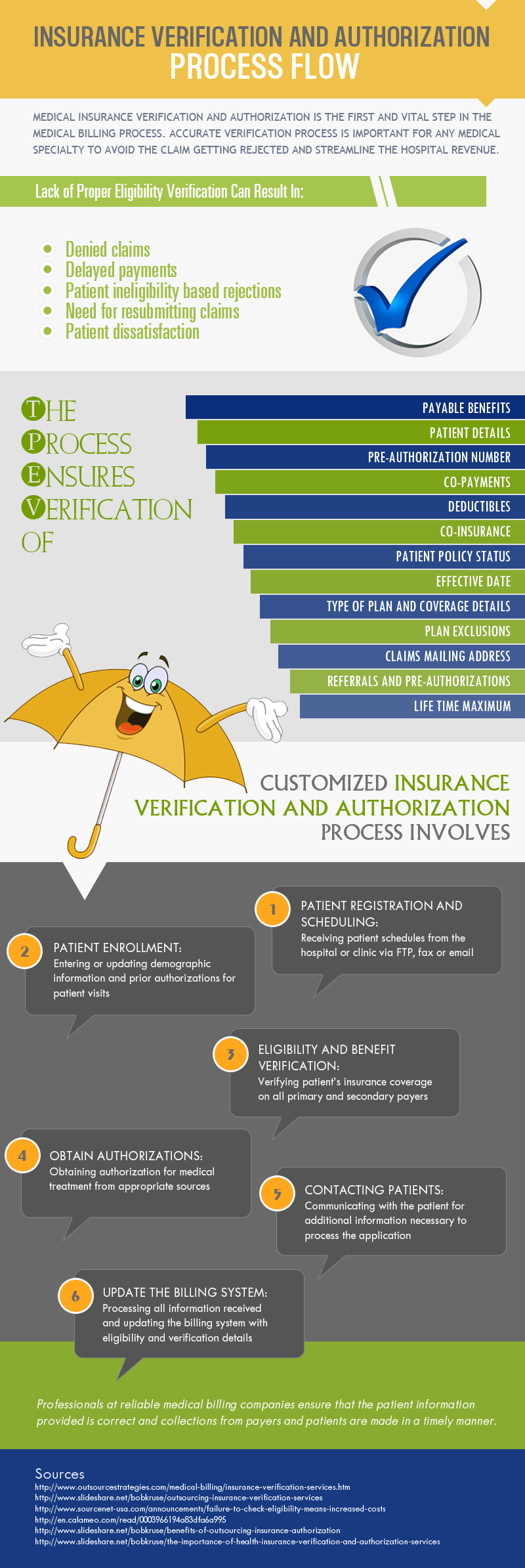
Insurance Verification and Authorization – Process Flow
Denied claims can become a huge waste of time and money for any practice. Insurance verification and authorization is crucial in accelerating physician’s reimbursement process.
Health insurance verification services involve checking the active coverage of the patients with the insurance company and related details. It plays a major role in the practice’s claim denial management program.
Even simple inaccuracies in patient information can lead to billing denials. The smallest details are important to getting medical bills paid the first time. Most of the claims get denied due to errors in eligibility. This happens because physicians and their practice staff have no way of knowing if a patient is eligible for coverage without verifying this information directly with the health insurance company.
An infographic presentation of the insurance verification process is given here.
Outsourcing your medical billing to GreenLeavez can save you up to 40% on your operational costs.
Call Our Toll-Free Number
GET YOUR FREE TRIAL TODAY!
